Federal vaccine guidance is changing. Here’s what that means for Americans.
Since the second Trump administration began earlier this year, federal health officials have amended national vaccine guidelines, sounded alarms about the alleged danger of vaccines and called for sweeping changes around vaccine regulation.
Several states have also introduced changes to vaccine policy. Illinois passed legislation empowering its Department of Public Health to set state vaccine guidelines rather than rely on federal guidance. Florida lawmakers are working to repeal and prohibit vaccine requirements for kids who attend public schools.
Amid nationwide shifts in vaccine policy, guidance and regulations, Straight Arrow News spoke with experts to understand current vaccine requirements, how changing federal guidance may impact Americans and what is on the horizon.
How does federal vaccine guidance translate into law?
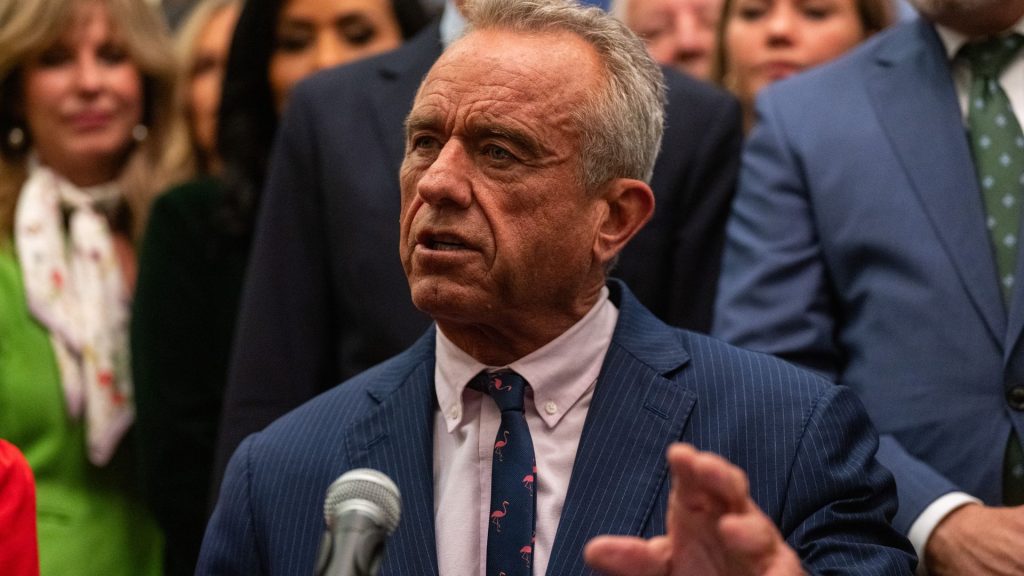
When Robert F. Kennedy Jr. took the helm as Health and Human Services Secretary, he promptly fired all 17 members of the Advisory Committee on Immunization Practices (ACIP), an independent group of physicians and public health officials that develops guidance about the use of vaccines in the country.
The newly constituted committee went on to change recommendations around the chickenpox vaccine, opting to separate it from the measles, mumps, and rubella vaccine. Earlier this month, ACIP also voted to change the longstanding practice of vaccinating all newborns against hepatitis B.
The same day ACIP made its hepatitis B recommendations, President Donald Trump signed an Executive Order directing Kennedy and the Centers for Disease Control and Prevention (CDC) to review vaccine recommendations from other developed countries and to amend the U.S. vaccine schedule to align with best practices, signaling more changes to come in 2026.
Typically, after ACIP votes on new guidance, the CDC director accepts or refuses it. Historically, the CDC has almost always accepted ACIP’s recommendations. The CDC approved both ACIP recommendations for new chickenpox and hepatitis B vaccination guidance.
But even if the CDC accepts the guidance, it is still just a recommendation. It is not a mandate, and it is not legally binding, Dorit Reiss, a professor of law at the University of California San Francisco, told SAN.
The federal government — outside of COVID-19 mandates and other rare historical disease outbreaks — does not make laws about who has to receive which vaccines. Instead, each state reviews federal recommendations and sets its own laws and vaccination schedules. Each state has its own procedures and statutes outlining how to utilize ACIP recommendations.
“Virginia empowers its Department of Health to make recommendations, and it refers to ACIP and says that the department will be guided by ACIP recommendation when it creates that, but they create their own,” Reiss said.
“No state automatically adopts ACIP recommendations into mandates. But some states do expressly refer to ACIP as the recommendation it should be guided by.”
Who is required to get vaccinated?
Today, no American, outside of the military, is required by law to receive any vaccine.
During the pandemic, this briefly changed when the Biden administration enacted several vaccine mandates, requiring COVID-19 shots for federal employees and contractors and health care workers who treated Medicare and Medicaid patients. The Department of Defense also mandated all servicemembers be vaccinated, and the U.S. Department of Labor’s Occupational Safety and Health Administration, or OSHA, required employers with more than 100 people to mandate vaccination or weekly COVID-19 testing.
These mandates faced a litany of legal challenges and were eventually all rescinded or blocked by courts.
Historically, there have been other rare moments when governments mandated vaccination, such as during a widespread measles outbreak in Philadelphia in 1991, according to Jason Schwartz, an associate professor in the Department of Health Policy and Management at the Yale School of Public Health.
But now that COVID-19 mandates have been cancelled, Americans are not required by any state or federal law to be vaccinated.
“We often talk about mandates or compulsory vaccination, but in no case is an individual or a child being vaccinated against their will or against their parents’ will,” Schwartz said.
Military personnel are an exception; they are required to receive certain vaccines depending on their specific occupation or where they deploy.
There are also state-level laws that require children to be vaccinated to attend public school.
“When we talk about these required mandates or vaccine mandates in the United States, it’s ultimately a policy in place that makes vaccination a condition of attending school in those states,” Schwartz told SAN.
“In all cases, public schools, sometimes those requirements apply to private schools or state-licensed daycare for younger children.”
Each state sets its own requirements for public school entry, and they differ significantly in the types of exemptions they allow. All states allow for medical exemptions, which permit children with certain health conditions, such as severe allergies, to skip vaccines and still attend public school.
Most states also allow for religious and philosophical exemptions, but that has shifted recently. In 2019, New York and Maine disallowed these exemptions. West Virginia long prohibited them, but earlier this year, the governor signed an executive order allowing religious exemptions. Earlier this month, the Supreme Court temporarily suspended the order.
States also differ in how parents apply for and receive these exemptions. In some states, parents check a box on a form to receive an exemption; in other states, schools hold review boards to ensure the exemption request is legitimate.
What might be at risk with future vaccine guidance changes?
One potential risk of future changes to federal vaccine guidance is insurance coverage. The Affordable Care Act requires all insurance companies to pay for any vaccines recommended by ACIP.
If ACIP stops recommending a vaccine — which it has not yet done— insurance companies would not have to cover it. Americans may have to pay for such vaccines out of pocket unless an insurance company, on its own volition, opted to continue covering them. Moreover, if the panel moved to stop recommending a vaccine altogether, then a federal CDC program called Vaccines for Children would no longer be able to purchase and distribute those vaccines to children on Medicaid or those without insurance.
“As of now, nothing that ACIP has done has lessened or weakened any of those financial coverage provisions because of how they’ve changed their recommendations quite deliberately, I think, to keep that access in place,” Schwartz said.
The post Federal vaccine guidance is changing. Here’s what that means for Americans. appeared first on Straight Arrow News.